Cardiology
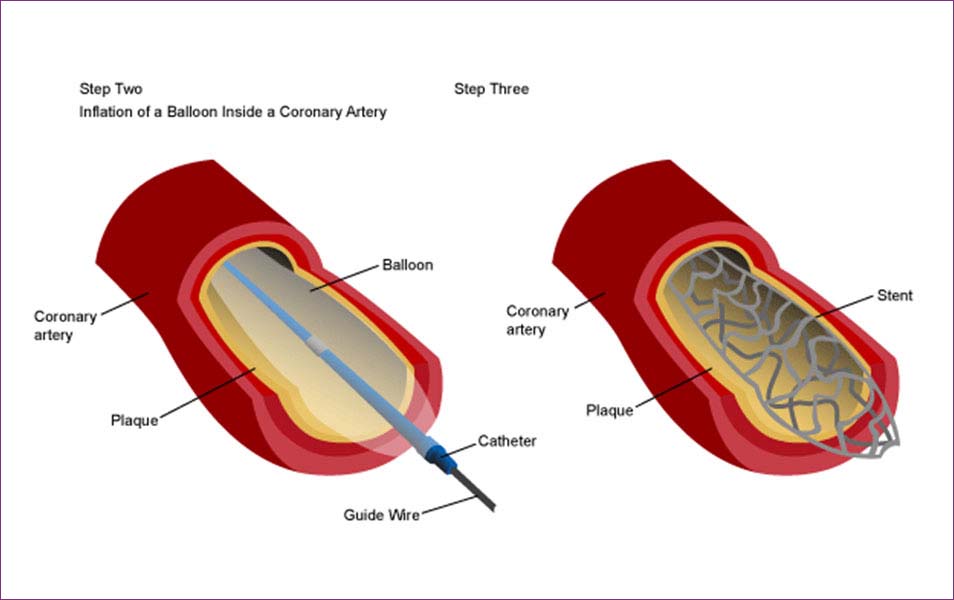
Coronary angiography & angioplasty.
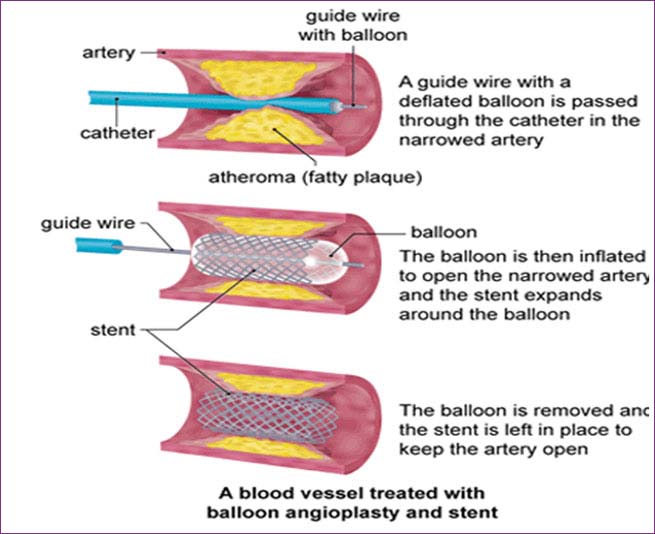
Coronary artery disease is a condition caused when a buildup of plaque, consisting of fatty deposits, cholesterol and calcium, stick to the walls of the arteries. This causes narrowing and blockages of the heart arteries, reducing the blood flow to the heart. This in turn may cause clots that can result in a heart attack. The main risks factors for coronary artery disease are:
Drug eluting, bare metal & absorbable stent implantation.
A drug-eluting stent (DES) is a peripheral or coronary stent (a scaffold) placed into narrowed, diseased peripheral or coronary arteries that slowly releases a drug to block cell proliferation.This prevents fibrosis that, together with clots (thrombi), could otherwise block the stented artery, a process called restenosis. The stent is usually placed within the peripheral or coronary artery by an interventional cardiologist or interventional radiologist during an angioplasty procedure.
Drug-eluting stents in current clinical use were approved by the FDA after clinical trials showed they were statistically superior to bare-metal stents for the treatment of native coronary artery narrowing’s, having lower rates of major adverse cardiac events (usually defined as a composite clinical endpoint of death + myocardial infarction + repeat intervention because of restenosis).
Primary angioplasty with clot removal in acute MI
The main purpose in case of the acute myocardial infarction is the resumption as fast as possible of the blood flow at the level of the obstructed coronary artery responsible for the production of the myocardial infarction. This may be accomplished by pharmaceutical or mechanical methods.
The primary angioplasty is the most efficient therapeutic method and is considered by the specialization forums as the method of choice in the treatment of acute myocardial infarction intended to decrease the death rate and the rate of complications. The most important aspect is the time elapsed from the onset of the chest pain and until the resuming of the circulation in the affected vessel. The faster is performed the surgery, the greater the quantity of saved muscle („time means muscle”).
The technique used is similar to percutaneous angioplasty and – depending on the case – adjuvant techniques may be used, such as thrombus aspiration (blood clot removal from coronary artery lumen), administration of drugs that prevent cell aggregation and blood clot formation, as well as the use of devices intended to facilitate the activity of the heart (intra aortic balloon counter pulsation).
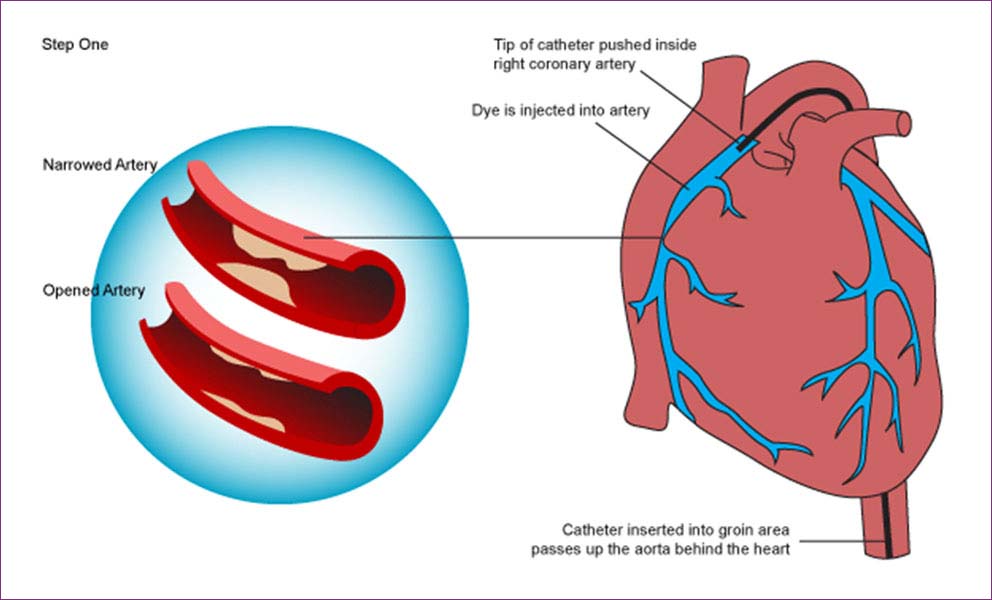
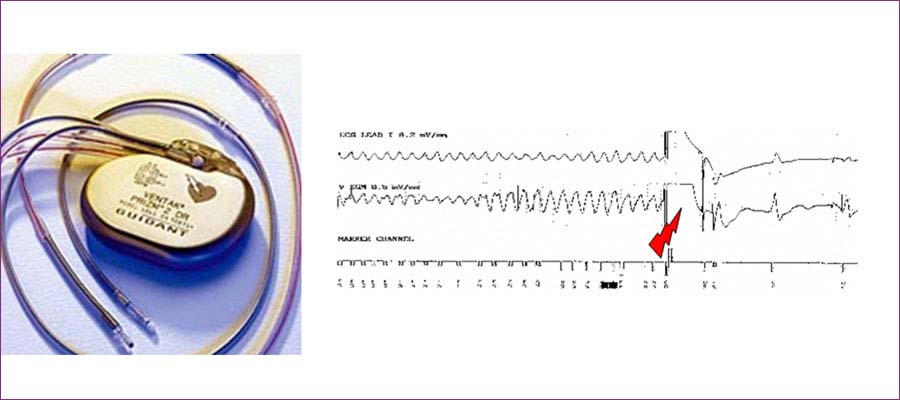
Pacemakers, AICD & CRT, Dim plantations, EP study & RF Ablation.
A pacemaker's is a medical device used to regulate the heart rate and to keep it from beating too slowly. Therefore, the most common indication for a pacemaker in a patient is slow heartbeat or heart block. Patients with atrial fibrillation and spells due to slow heart rate are also candidates for pacemaker implantation. The latest indication for pacemaker is cardiac resynchronization therapy for pacing with congestive heart failure.
A pacemaker system consists of the "pulse generator" and the "lead." The pulse generator is where the battery and the electronics reside. It is the "brain" of the pacemaker. It is connected to a "lead," or a wire, through which the "brain" of the pacemaker communicates with the heart. The connection between the lead and the pulse generator is called the "header."
Most pacemakers in use today are "dual chamber" pacemaker because they utilize two electrodes, which are placed respectively in the atrial and ventricular chamber, thus "dual chamber." (See anatomy and physiology section). The advantage of such a system is that is preserves the normal physiology of the heart, i.e., normal relationship between the upper chamber and lower chamber. A "single chamber" pacemaker uses only one electrode, which can be placed in either the atrium or the ventricle. A single chamber pacemaker is less frequently used in the U.S. because it does not preserve the normal relationship between the upper and lower chambers of the heart. A single chamber pacemaker is most commonly used when such a normal relationship is no longer present in patients with chronic atrial fibrillation.
During surgical implantation of the pacemaker system, the leads are inserted through the vein on the chest. They are subsequently placed permanently inside the chambers of the heart whereas the "pulse generator" itself is implanted on the chest just under the skin (subcutaneous) because the procedure is done transvenously (through the vein), it does not require an open heart surgery. This surgery can be completed in as short as 20 minutes and is associated with reasonably low risks and rapid recovery (see also frequently asked questions section).
Major complications are rare but may include cardiac perforation, pneumothorax (air leak in the lung), vascular injury, and hematoma (blood clot). Infection of the pacemaker may occur in 1 percent of the time which will require explantation of the entire pacemaker system.
While older generations of pacemaker has only one function and that is pacing the heart, newer generations of pacemakers have the added capability of cardiac resynchronization therapy (CRT). They can be used in patients without slow heartbeat but who suffer from heart failure refractory to standard medical therapy.
Implantable Cardioverter Defibrillator (AICD or ICD)
A defibrillator is a medical device whose primary function is to shock the heart when the heart has gone into a very rapid and life-threatening arrhythmia such as ventricular tachycardia. Its secondary function is to pace the heart when the heart rate is too slow.
A frequent question that comes up is whether a particular device is a "defibrillator" or a "pacemaker" or a "combination." A pacemaker simply paces the heart when it is too slow. It has no defibrillator function, i.e., it cannot "shock" the heart in the case of an emergency. A defibrillator, on the other hand, can pace the heart when it is too slow, and shock the heart when it is too fast. All defibrillators today can also work as pacemakers, and therefore the concept of a "combination" pacemaker-defibrillator is no longer relevant. There are no defibrillators today that work only as a "shock box" without full pacemaker capability. The converse, however, is not true.
A defibrillator is used to treat patients with life-threatening arrhythmias. When first invented in the 1980s, defibrillators were reserved for patients who have already suffered a cardiac arrest or have documented serious arrhythmias. However, most defibrillators today are implanted on a prophylactic basis, i.e., preventatively. In other words, they are implanted in patients at high risk for a serious arrhythmia and cardiac arrest but who have not yet suffered such an event. While this idea may be difficult for some patients and even some physicians to accept, prophylactic defibrillator implantation is no different, conceptually, than treating hypertension or hypercholesterolemia for prevention of heart attack. One does not wait for cardiac arrest to occur before implanting a defibrillator, just as one does not wait until a full blown heart attack to take place before treating patient's elevated blood pressure and cholesterol. Current recommendation is for defibrillator implantation in patients with an ejection fraction less than 35%.
The anatomy of a defibrillator is very similar to that of a pacemaker, except that the size of the pulse generator and the electrodes are significantly bigger and the structures more complicated. This is because the defibrillator needs to deliver higher energy to shock the heart than what is required to pace the heart. The placement of the electrodes inside the heart is also more critical that that for the pacemaker because the effectiveness of the "shock" function depends greatly on the location of the electrodes.
Similar to pacemakers, defibrillators are inserted transvenously (through the vein) and therefore do not require an open heart surgery. Surgical risks are similar to those with pacemaker
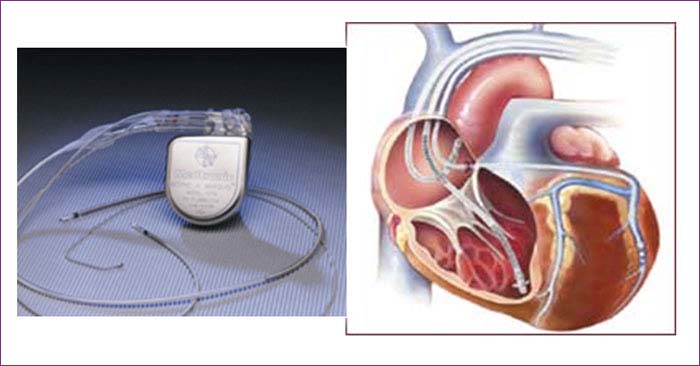
Cardiac Resynchronization Therapy (CRT).
This is a percutaneous (through the skin) surgical procedure specifically for the treatment of patients with severe congestive heart failure. In patients with heart failure, the left ventricle is enlarged and the time it takes to activate the entire heart may be significantly increased, leading to "dyssynchrony," or lack of synchronized or coordinated contraction of the heart. This usually manifests itself as abnormal EKG with either right bundle branch block or left bundle branch block. The larger the heart and the greater the degree of dyssynchrony (as assess by echocardiogram and EKG), the more one would benefit from CRT. CRT works by pacing both the right and left side of the heart simultaneously, shortening the time to activate the heart and restoring "synchrony" to the heart, thus the term "Cardiac Resynchronization Therapy (CRT)."
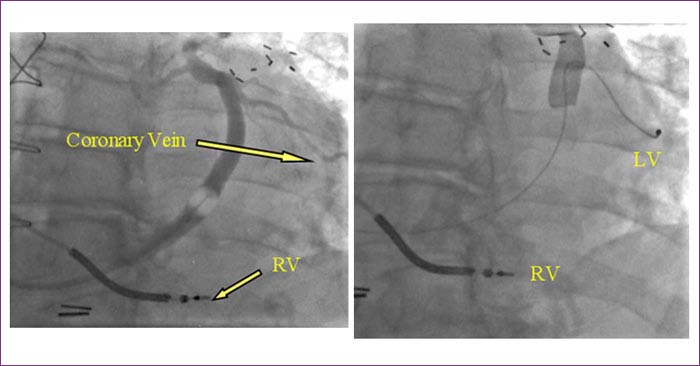
A CRT device can be a CRT pacemaker or a CRT defibrillator. Most CRT devices implanted in the U.S. are the defibrillator type because most patients with heart failure who need CRT will also need a defibrillator. A CRT device works by having a "third wire" capability to pace the left side of the heart.
Ordinary pacemakers and defibrillators come with two wires, one in the right atrium and one in the right ventricle (RV). CRT pacemakers and defibrillators have an extra wire which goes into the left ventricle (LV), via a vein in the back of the heart called "coronary sinus." The branches of the coronary sinus are called "coronary veins," through which the "third-wire" is placed in order to pace the left side of the heart (see diagram below). Simultaneous pacing of both right and left ventricle can be performed through these wires in order to "resynchronize" the heart. This can result in dramatic improve symptoms of heart failure for those patients with heart failure and dyssynchrony. Most patients with CRT implantation will experience improvement in their breathing, stamina, and exercise capacity. The ejection fraction and other important parameters of the heart may also improve.
For a CRT defibrillator, the CRT portion of the device is an added feature of the unit. In other words, the device can provide CRT while still functioning as a defibrillator. A standard two-wire defibrillator works as a defibrillator without CRT function.
Although CRT has been available since the late 1990s, it has only recently gained wide-spread acceptance and popularity following the publication of several large landmark clinical trials which demonstrated significant improvement in heart failure patients who have received CRT. Today, CRT is considered a standard of care for patients with heart failure and evidence of dyssynchrony, who continue to have refractory symptoms of heart failure despite optimal medical treatment.
Risks of the surgery is similar to those of the pacemakers and standard defibrillators. The additional "third wire" placed in the left side of the heart used to be a critical step that was difficult to achieve and took many hours. Today, with improved technique and equipment, the deployment of the "third wire" for CRT may take as few as an extra 10 minutes compared to the standard pacemaker or defibrillator.
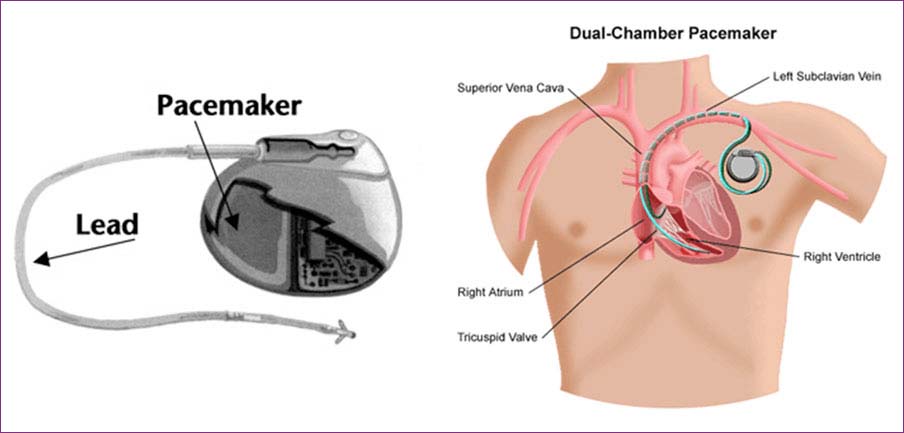
Electrophysiology study (EPS).
This invasive study is generally needed for patients whose causes for fainting or severe palpitation remain unknown despite extensive noninvasive evaluations. It is also useful to differentiate the various causes for a documented episode of arrhythmia. It can be used to risk-stratify certain patients with known or suspected arrhythmias. Lastly, it is performed in conjunction with radiofrequency ablation, as a mean to confirm the mechanism of the arrhythmia before performing curative ablation.
The procedure is performed in a hospital setting in the cardiac catheterization laboratory, the same facility where coronary angiogram and angioplasty are performed. Under sedation, lidocaine (or equivalent local anesthetics) is injected into the skin. Several catheters are then inserted into veins in the groins and into the heart (see picture), after which electrical stimulation of the heart is performed through these catheters by the Electro physiologist. This electrical stimulation can reveal an underlying electrical conduction problem such as slow heartbeat or heart block, as well as reproducing and confirming the cause of a rapid heartbeat. For patients with rapid heartbeat problem, they do not necessarily have to be in their arrhythmia at the time of the procedure since this test can "provoke" the dormant arrhythmia.
If a slow heartbeat is documented, one can prescribe the appropriate treatment, usually a pacemaker. If a fast heartbeat is confirmed, there are several treatment options, depending on the type of rapid heartbeat discovered. For some rapid heartbeat that are potentially life-threatening, such as ventricular tachycardia, an implantable defibrillator is required. On the other hand, for many other forms of rapid heartbeats, such as SVT, the arrhythmias can be "mapped" to determine the exact source of the problem, which is usually an "extra nerve" in the heart. In the majority of these cases, ablation can successfully eliminate the culprit of the arrhythmias, resulting in a long-term permanent cure for the patient.
Thus, an Electrophysiology study is a diagnostic study that helps the Electro physiologists confirm the root of the suspected electrical problem of the heart. It serves as a gateway to other therapeutic modalities available to treat the arrhythmias.
Many patients who have serious symptoms from their rapid heartbeat, such as fainting or near-fainting, may be very reluctant to have a test which can provoke their arrhythmias, for fear of reproducing the frightening sensation. Reproducing the arrhythmia, however, may be the only way to confirm the causes of their conditions in most patients. Furthermore, there is no safer place to have an arrhythmia than in the cardiac catheterization laboratory, under the direct care of a Cardiac Electro physiologist, and in the presence of an entire team of personnel specializing in the chronic as well as emergency treatment of arrhythmias. It is better to find it here than to have it occur "naturally" at home or while driving on the road.
In contrast to an coronary angiogram, which is a procedure designed to look for clotted arteries of the heart (coronary arteries), an Electrophysiology study is not meant to evaluate the patency of patient's arteries. But rather, it focuses on the evaluation of the electrical health of the heart. One, therefore, cannot tell "if the arteries are blocked" by this test. This is the job for your general or interventional cardiologists.
Radiofrequency ablation (RFA)
This is a cardiac procedure specifically designed to treat and cure certain types of arrhythmias (see sections on supraventricular tachycardia, Wolff-Parkinson-White Syndrome, and atrial flutter).
Ablation is a procedure of selectively destroying certain tissues of the body to cure or control a disease process. An ablation can be performed for seizure focus in the brain or for certain masses in the liver, or for abnormal electrical activities in the heart. Cardiac ablation refers to ablation specific to the heart rhythm problem. The most common source of energy for cardiac ablation is radiofrequency and thus the most common term for this procedure is "radiofrequency ablation," although other sources of energy have been used.
For cardiac ablation, very thin catheters are placed into the heart via large veins in the groin and sometimes in the neck (see picture above). This is why the procedure is also called "trans-catheter ablation," to distinguish it from open-heart surgical ablation. The procedure is done much like that of an Electrophysiology study, which is first performed to identify the source of the arrhythmia. "Mapping" is done to localize the source of the problem, after which ablation is performed targeting and selectively destroying the areas that are responsible for the arrhythmias.
For the purpose of discussion on this website, the term "radiofrequency ablation" means cardiac ablation procedures performed "percutaneous," or "endocardially" through a catheter (trans-catheter). In other words, they are performed by a minimally invasive technique via a vein or artery through the skin (percutaneous), not by an open-chest or open-heart surgery. The approach is from inside the heart (endocardial), because the catheters enter the heart on the inside, as opposed to outside the heart (epicardial) as in open-heart surgery. In the latter case, the approach is through a surgical opening in the chest and these epicardial ablation procedures are done by cardiothoracic surgeons, not by Cardiac Electro physiologists.
Cure rates for most forms of arrhythmias by radiofrequency ablation range form 80% to 98% (please see sections on specific arrhythmias for individual discussion). Complications rates are low, with mortality less than 1 in several thousand and very small risks of bleeding and perforation.
For many types of arrhythmias, radiofrequency ablation is increasingly accepted as an preferred therapeutic alternative to chronic therapy with medications. It is considered first-line therapy for most curable arrhythmias such as supraventricular tachycardia, Wolff-Parkinson-White Syndrome, and atrial flutter.
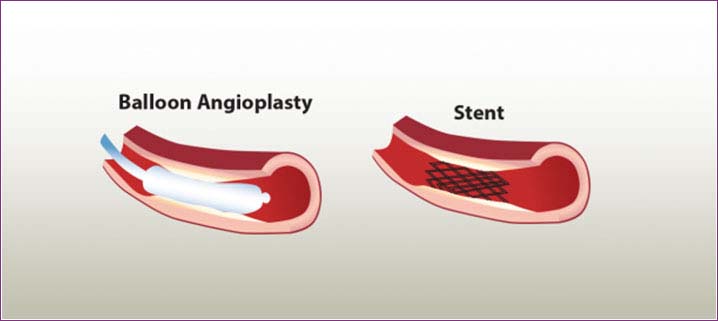
Balloon Mitral valvuloplasty & PBPU & PBAV.
This balloon valvotomy procedure can be performed on the mitral, tricuspid, aortic or pulmonary valves. Balloon valvotomy is a non-surgical procedure performed in the cardiac catheterization laboratory by a cardiologist and a specialized team of nurses and technicians.Long, slender tubes called catheters are first placed into blood vessels in the groin and guided into the chambers of the heart. The cardiologist then creates a tiny hole in the wall between the upper two chambers of the heart. This hole provides an opening for the cardiologist to access the left atrium with a special catheter that has a balloon at the tip.
The catheter is positioned so the balloon tip is directly inside the narrowed valve. The balloon is inflated and deflated several times to widen the valve opening. Once the cardiologist has determined that the opening of the valve has been widened enough, the balloon is deflated and removed.
During the procedure, the cardiologist may perform an echocardiogram (ultrasound of the heart) to get a better picture of the mitral valve.
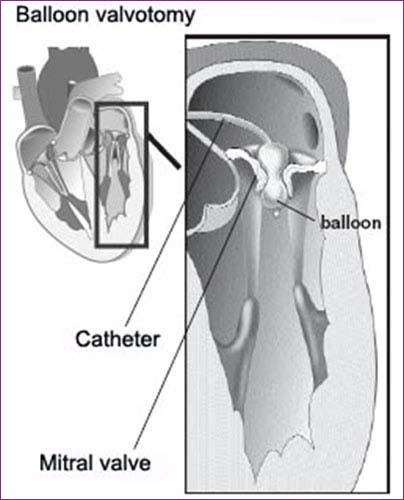
Balloon valvotomy is a procedure that may relieve many of the symptoms of valve disease, but it will not cure valve disease. Some patients may continue to need medications, even after a successful procedure.
After the procedure, you will need to continue seeing your doctor regularly to make sure your heart valves are working properly. Lifestyle factors that can worsen valve disease may also need to be changed. An exercise program may be prescribed to improve your heart health after the procedure.
To protect your heart valves from further damage, tell your doctors, dentist and other health care providers that you have valve disease so antibiotics can be prescribed before you undergo any procedure that may cause bleeding. Also, take good care of your teeth and gums.
PREFABRICATED BEDSIDE PATIENT UNIT (PBPU)
PBPU is provided adjacent to each single bed and between each pair of beds for the listed areas. PBPU Style B1 and B2 (Recovery): This unit is for patients who donot require physiological monitoring and shall be provided for adesignated percentage of the beds in Respiratory Care Units and for each bed in Surgical Recovery Facilities. This PBPU is provided foreach bed and contains medical gas and vacuum outlets in the Intensive care configuration.
PBPU Style C: This unit is provided for each bed in all IntensiveCare Units, the Life Support Unit in Ambulatory Care, and a designatedpercentage of the beds in the Respiratory Care and Spinal Cord InjuryUnits. It contains all of the required services for Intensive Care,including physiological monitoring capability.
Pediatric Cardiac Catheterization
Cardiac catheterization is a minimally invasive procedure that entails inserting a thin, flexible tube (catheter) through a vein or artery which is then guided to the heart. Physicians perform this study to diagnose the type of heart defect and its severity. In some cases, they are also able to repair the heart problem (congenital or acquired) that might otherwise have required surgery.
Benefits of Cardiac Catheterization
Because cardiac catheterization procedures are less invasive than open surgery, they are inherently associated with fewer risks. Newborn babies with congenital heart defects benefit greatly from catheter-based procedures either to diagnose or treat these problems. Other advantages of these interventional procedures include: shorter hospital stays, quicker recovery time and less discomfort and scarring than conventional heart surgery.
IABP, Pericardiocentesis
Intra-aortic balloon pump
Cardiogenic shock or acute heart failure can represent a life-threatening situation that requires immediate circulatory support. The intra-aortic balloon pump can save the patient's life by providing temporary support to the heart.
An intra-aortic balloon pump (IABP) is a device that supports the heart in pumping a sufficient amount of blood around the body. The IABP is implanted into the patient's aorta.
This device consists of a balloon firmly mounted on a catheter.
It is available round-the-clock to provide emergency cardiovascular support. Insertion of the device only takes a matter of minutes, and does not cause any pain. The procedure, which involves the insertion of the catheter via an artery in the groin, can be performed either in the catheterization laboratory or in the intensive care unit. Only a local anesthetic is required, which will be applied to the groin area.
Using x-ray guidance, the balloon is then positioned at chest height inside the aorta.
The balloon inflates and deflates in time with the patient's heartbeat, providing support to the heart and improving organ perfusion.
Pericardiocentesis
Pericardiocentesis is a procedure that uses a needle to remove fluid from the pericardial sac. This is the tissue that surrounds the heart.
The procedure is most often done in a special procedure room, such as a cardiac catheterization laboratory. It may also be done at a patient's hospital bedside. A health care provider will put an IV into your arm in case fluids or medicines need to be given through a vein. For example, you may be given medicines if your heartbeat slows or your blood pressure drops during the procedure.
The health care provider will clean an area just below the breastbone or below the left nipple. Numbing medicine (anesthetic) will be applied to the area.
The doctor will then insert a needle and guide it into tissue that surrounds the heart. Often, echocardiography is used to help the doctor see the needle and any fluid drainage. An electrocardiogram (ECG) and x-rays (fluoroscopy) may also be used to help with positioning.
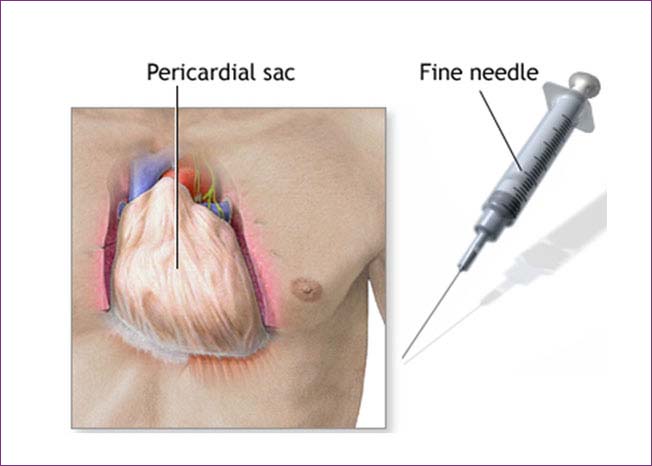
Once the needle has reached the correct area, it is removed and replaced with a tube called a catheter. Fluid drains through this tube into containers. Most of the time, the pericardial catheter is left in place so draining may continue for several hours.
Surgical drainage may be needed if the problem is hard to correct or comes back. This is a more invasive procedure in which the pericardium is drained into the peritoneal (abdominal) cavity. This may need to be done when you are under general anesthesia.
ECG, Echocardiography with 3Dimaging
Echocardiography (ECG) – Capturing Your Heart
With the advancement of technology, knowing your heart is not that difficult anymore. Sophisticated scanning and imaging techniques can tell you the shape, size, and condition of your heart in no time at all. Echocardiography is one such imaging technique which gives you a fair idea about how well your heart is functioning. And yes, echocardiography is painless.
What is Echocardiography (ECG)?
Echocardiography (echo = sound + cardio = heart + graphy = study) is a painless medical procedure that creates moving images of the heart with the help of sound waves. Echocardiography helps you to know the shape, size and functioning of the valves and chambers of your heart.
An echocardiography can accurately mark areas of the heart muscle that are not contracting well. The reasons may be poor blood flow, or an injury from a previous heart attack. Doppler Ultrasound, a type of echocardiography, can show how well the blood flows through the chambers and valves of your heart.
Other features of echocardiography (ECG) include –
Different types of Echocardiography (ECG)
There are different types of echocardiography. However, all of them use sound waves to create moving images. Unlike x-ray and some other screening tests, no radiation is involved in this procedure.
Transthoracic Echocardiography
This is the most common form of echocardiogram. It is a noninvasive procedure, which means that no instruments are inserted inside the body to perform the test.
Transthoracic echo involves placing a device called a ‘transducer’ on the chest of the patient. The device sends ultrasound waves through the chest wall, inaudible to human ear. As the sound waves hit the heart and bounce off the structure of the heart, the echo machine converts them and projects the image on a screen.
Stress Echocardiography
Stress echocardiogram is a part of the stress test, performed to see the functioning of the heart under stress. During this test, initially, images of your heart are taken at a resting position. Then using a machine, usually a treadmill, you are required to increase your heart beat, after which another set of images are taken. Finally, both are compared to obtain results.
Stress echocardiography can detected the presence of coronary artery disease (CAD). It is supposed to be performed in the presence of a licensed practitioner, such as a cardiologist and cardio sonographer.
Transesophageal Echocardiography
It may be that your doctor is unable to obtain clear images of your aorta and other parts of the heart from a Transthoracic Echocardiography. In that case, a Transesophageal Echo is performed, wherein the transducer is placed at the end of a tube and passed down your throat into the oesophagus, the passage from your mouth to your stomach. This helps the doctor to obtain images from a location directly behind the heart.
Three-Dimensional Echocardiography
3D Echocardiography (also known as 4D Echocardiography when the image is moving) creates three dimensional images of the heart. This type of echocardiography helps the doctor to take a look at the heart from all sides in real time. This procedure is used to see those type of hearts that are malformed during the time of birth.
What to expect before, during and after an Echocardiography (ECG)
Who should take an Echocardiography (ECG)?
Anyone above the age of 30 should undergo echocardiography as part of a preventive health checkup. Considering the impact of NCDs/ lifestyle diseases and the nature of a heart attack, which often happens without a warning, a timely echocardiography can tell you the status of your heart in great detail.
DSE, TEE, TMT, HUTT & Holter monitoring
Holter monitor
It is a machine that continuously records the heart's rhythms. The monitor is worn for 24 - 48 hours during normal activity.
How the Test is Performed
Electrodes (small conducting patches) are stuck onto your chest. These are attached by wires to a small recording monitor. You carry the Holter monitor in a pocket or pouch worn around your neck or waist. The monitor runs on batteries.
While you wear the monitor, it records your heart's electrical activity.
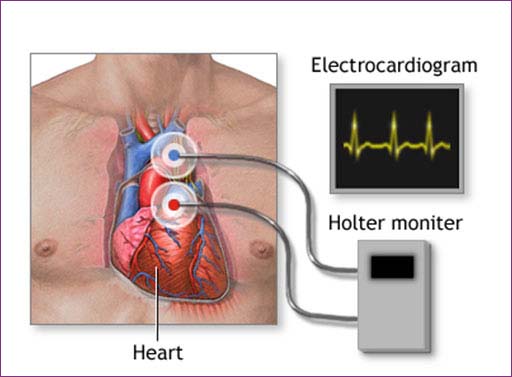
It is very important that you accurately record your symptoms and activities so the doctor can match them with your Holter monitor findings.
Electrodes must be firmly attached to the chest so the machine gets an accurate recording of the heart's activity.
While wearing the device, avoid:
Continue your normal activities while wearing the monitor. You may be asked to exercise while being monitored if your symptoms have occurred in the past while you were exercising.
Head Up Tilt Table (HUTT)
A HUTT is used to determine the cause of fainting spells. The test involves being tilted, always with the head-up, at different angles for a period of time.
Heart rhythm, blood pressure and other symptoms are closely monitored and evaluated with changes in position. The patient is completely conscious for the test and an intravenous line is placed prior to the exam. This is an outpatient procedure.
TMT
TMT stands for Tread Mill Test.
It is a screening tool to test the effect of exercise on the heart.
In this test patient is made to walk on a treadmill and electrical activity of the heart is measured with an ECG, and blood pressure recordings are taken every few minutes. As per a standard protocol patient is made to walk till target heart rate is reached, but if the patient develops chest discomfort or ECG changes the test is terminated.
The test is indicated:
TEE
Transesophageal echocardiography (TEE) is a test that produces pictures of your heart. TEE uses high-frequency sound waves (ultrasound) to make detailed pictures of your heart and the arteries that lead to and from it. Unlike a standard echocardiogram, the echo transducer that produces the sound waves for TEE is attached to a thin tube that passes through your mouth, down your throat and into your esophagus. Because the esophagus is so close to the upper chambers of the heart, very clear images of those heart structures and valves can be obtained.
Quick facts
TEE is a test that uses sound waves to make pictures of your heart’s muscle and chambers, valves and outer lining (pericardium), as well as the blood vessels that connect to your heart.
DSE
DOBUTAMINE STRESS ECHOCARDIOGRAPHY (DSE)
A dobutamine stress echocardiogram is a diagnostic procedure that may be used when a doctor wants to assess the heart muscle under stress. If exercise on a treadmill is not an option (too much stress on the heart) due to a person’s medical condition, a doctor may use an intravenous medication called dobutamine. Dobutamine causes the heart to beat faster and will mimic the effects of exercise on the heart.
An echocardiogram is a noninvasive (the skin is not pierced) procedure used to assess the heart's function and structures. During the procedure, a transducer (like a microphone) sends out ultrasonic sound waves at a frequency too high to be heard. When the transducer is placed on the chest at certain locations and angles, the ultrasonic sound waves move through the skin and other body tissues to the heart tissues, where the waves bounce or "echo" off of the heart structures. The transducer picks up the reflected waves and sends them to a computer. The computer displays the echoes as images of the heart walls and valves.
A dobutamine stress echocardiogram may utilize one or more of four special types of echocardiography, as listed below:
M-mode echocardiography - This, the simplest type of echocardiography, produces an image that is similar to a tracing rather than an actual picture of heart structures. M-mode echo is useful for measuring heart structures, such as the heart's pumping chambers, the size of the heart itself, and the thickness of the heart walls.
Doppler echocardiography - This Doppler technique is used to measure and assess the flow of blood through the heart's chambers and valves. The amount of blood pumped out with each beat is an indication of the heart's functioning. Also, Doppler can detect abnormal blood flow within the heart, which can indicate a problem with one or more of the heart's four valves or with the heart's walls.
Color Doppler - Color Doppler is an enhanced form of Doppler echocardiography. With color Doppler, different colors are used to designate the direction of blood flow. This simplifies the interpretation of the Doppler technique.
2-D (two-dimensional) echocardiography - This technique is used to visualize the actual structures and motion of the heart structures. A 2-D echo view appears cone-shaped on the monitor, and the real-time motion of the heart's structures can be observed. This enables the doctor to see the various heart structures at work and evaluate them.
Renal angioplasty
A renal angioplasty is a procedure used to widen the arteries that supply blood to your kidneys (your renal arteries). You may be offered this procedure if you have a condition called renal artery stenosis, which is when your renal arteries become very narrow.
Peripheral Angioplasty
Peripheral artery disease also referred to as peripheral arterial disease, is a common circulatory problem in which narrowed arteries reduce blood flow to the lower extremities (legs).
When a person develops peripheral artery disease (PAD), the extremities — usually the legs — don't receive enough blood flow to keep up with the body’s needs. This causes symptoms, most notably leg pain when walking (intermittent claudication).
Peripheral angioplasty is a minimally invasive procedure. These procedures are performed in a cardiovascular catheterization laboratory, under local anesthesia. An IV (intravenous line) into the arm or hand will provide medication to make the procedure as comfortable as possible. A catheter is inserted into a blood vessel in the upper thigh (groin). Using high-resolution fluoroscopic (X-ray) video and film equipment, the catheter is guided through to the peripheral artery that is being treated. Once the catheter is in place the balloon is inflated and the narrowed peripheral artery is stretched open. The fatty plaque or blockage is pressed against the peripheral artery walls enlarging the diameter of the peripheral artery. After the blocked area of the peripheral artery is widened the balloon is deflated and removed. Blood flowing through the peripheral artery is increased, supplying blood to the heart.
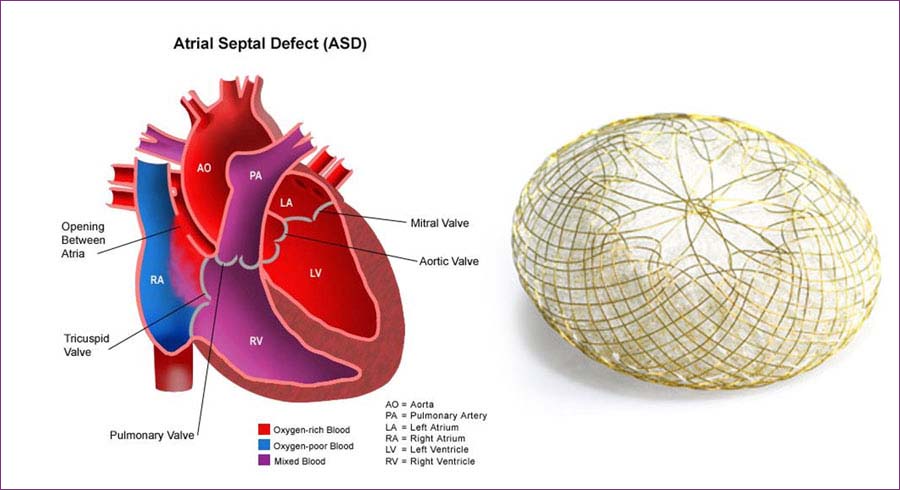
Device closure of ASD, PDA
ASD
PDA is a congenital abnormality of the heart in which blood is shunted from the aorta (high pressure vessel) through the ductus arteriosus into the pulmonary artery (lower pressure vessel) resulting in fluid build-up in the lungs.
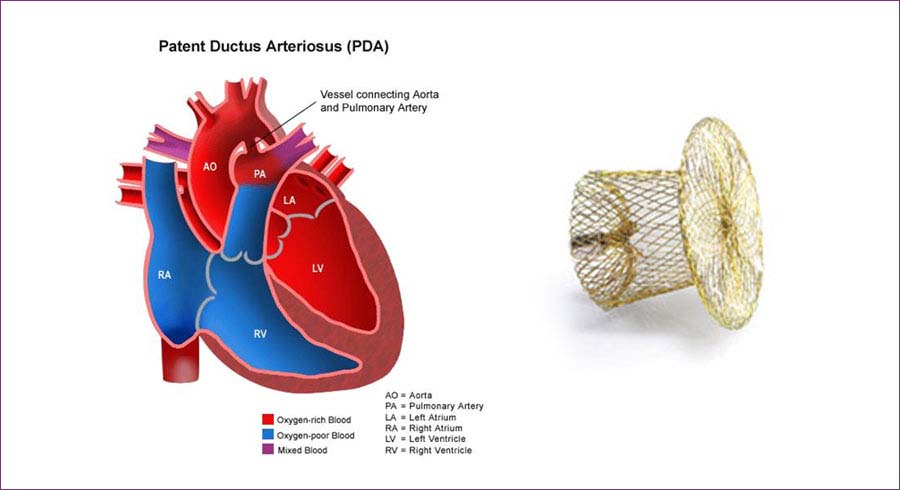
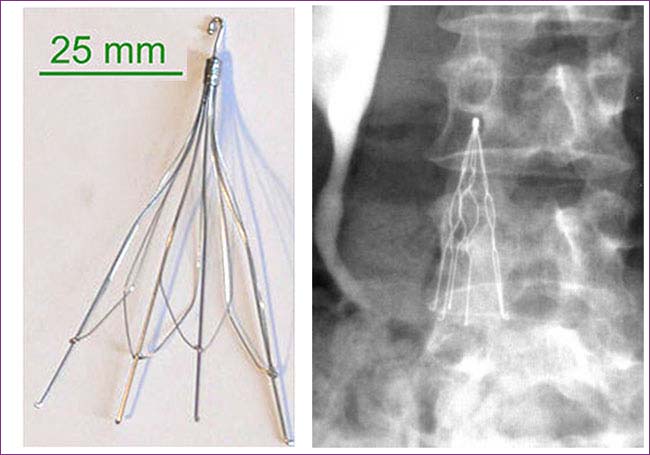
The device is made of braided Nitinol threads. Nitinol is a very elastic metal with wide-ranging memory skills. Each PDA consists of an aortic disc connected to a conical-shaped shank. To accommodate different PDA anatomies, the PDA is available in several sizes, each with either a standard (short), or long shank. Polyethylene (PET) patches inside the device support immediate closure of the defect.
PDA
The ASD device used to close an ASD defect. The device is made of braided Nitinol threads. Nitinol is a very elastic metal with wide-ranging memory properties. The device consists of two discs with a larger intermediate waist. Inside each of the discs there is a Polyethylene (PET) patch, to support the immediate closure. This helps stop the blood going through the meshwork of the device. The device will be pushed through the delivery catheter across the defect, then both discs will fix the device at the septum wall and the device will then be released when placed in the correct position to close the defect.
IVC Filter for prevention of PTE
Inferior vena cava (IVC) filter placement is most commonly indicated for deep venous thrombosis (DVT) or pulmonary embolism (PE) when anticoagulation therapy is contraindicated.